Tips from the Experts
Sciatica
Millions of people suffer from low back pain each day. Most are between the ages of 30 and 50, and many endure not only back pain, but also severe pain or numbness running into one or both legs. The result: loss of activity, inability to work and inability to participate in the activities we enjoy most. It is estimated that some 80 to 90% of Americans will suffer from back pain during their lifetime, about 50% of which will have more than one episode. Often times, you will hear the name “Sciatica” associated with this pain, and rightly so.
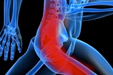
Millions of people suffer from low back pain each day. Most are between the ages of 30 and 50, and many endure not only back pain, but also severe pain or numbness running into one or both legs. The result: loss of activity, inability to work and inability to participate in the activities we enjoy most. It is estimated that some 80 to 90% of Americans will suffer from back pain during their lifetime, about 50% of which will have more than one episode. Often times, you will hear the name “Sciatica” associated with this pain, and rightly so.
The lay term sciatica is frequently misused and its definition often misunderstood. Sciatica is actually the name designated to the symptoms rather than the diagnosis itself. Sciatica, or radiculopathy, is a general term that refers to pain radiating into the leg caused by compression or irritation of one or more nerves exiting the lower spine. These nerve roots together form the sciatic nerve. Sciatica, or sciatica-type pain is often intermittently deep and steady, and can usually be reproduced with certain activities and positions, such as sitting or walking. Pain can be accompanied by numbness and tingling, muscle weakness and loss of specific reflexes. Often times the leg pain, which may correspond to the specific nerve root that is compressed, will be much worse than the low back pain.
There are a number of different conditions that can cause compression, irritation and inflammation of the spinal nerves. Some of these include herniated discs, stenosis which is the narrowing of the hole through which the spinal nerve exits due to bone spurs or arthritis, piriformis syndrome, degenerative disc disease, spondylolisthesis, nerve root injuries and scar tissue from previous spinal surgeries. Although a traumatic event may accompany the onset of pain, it is more common for the pain to develop as a result of general ‘wear and tear’ of the lower spine.
The clinical diagnosis for the cause of Sciatica is usually arrived at through a combination of the patient’s history (including description of pain) and a physical exam. Imaging studies such as MRIs and CT-myelograms are sometimes ordered by your physician and may be used to confirm the diagnosis. Most often these tests may be performed 3-4 weeks into the painful exacerbation. Identification of the cause of your symptoms is critical in alleviation of the pain as treatments my vary.
Luckily, most flare-ups heal quickly within a few days or weeks and respond well to rest, ice/heat at 20 minute intervals, and NSAIDs initially. However, often a more structured pain management and therapeutic training program is necessary which may include exercise, stretching, acupuncture, massage or manual manipulation.
While it may seem counterintuitive, exercise is usually better for healing sciatic pain than bed rest. When symptoms are at their worst, most physicians recommend rest for a day or two, but resting for longer periods of time is usually not advisable. Without exercise and movement, the back muscles and spinal structures become deconditioned and less able to support the back. Deconditioning and weakening can lead to further back injury and strain, which causes additional back pain. In fact, inactivity may even make your sciatic pain worse. This is because regular movement and exercise is necessary to nourish the various structures in the low back and encourage the strength needed to support the low back.
Once you are on your feet it is critical to identify what particular movements which improve your leg symptoms, and which movements or postures worsen them. Although this may just seem a little too easy, promoting pain reduction posturing is key to reducing the nerve irritation and thus the pain. For instance, if you experience pain in the leg when sitting for a period, and standing and walking relieves those symptoms, then try to stand and walk whenever possible. Conversely, if sitting eliminates the pain in the leg caused by ambulation, bias your activity towards sitting. What you have just determined is your potential treatment bias of flexion (sitting, bending, gentle knees to chest) or of extension (standing, walking, gentle backward bending). To be effective, the activities and postures recommended for ones pain management must be done regularly.
Close attention daily to one’s posture and body mechanics is the key to getting maximum benefit during daily activities and from exercise. Continuing with a program of gentle exercise focusing on abdominal and back strengthening, lower extremity stretching, along with walking or swimming is beneficial for both management of the current episode of pain and for overall back health and prevention of future back problems.
If you or someone you know suffers from pain as described above, it is ill-advised to begin a new exercise program without consulting first with your Physician, a physical therapist, certified athletic trainer, chiropractor, physiatrist or other spine specialist who regularly treats low back pain and leg pain associated with sciatica. It is important to first get an accurate diagnosis for the cause of sciatic pain, as the specific exercises recommended will depend on the cause of the sciatica.
