Rehab Articles
Juvenile Arthritis
What is juvenile arthritis?
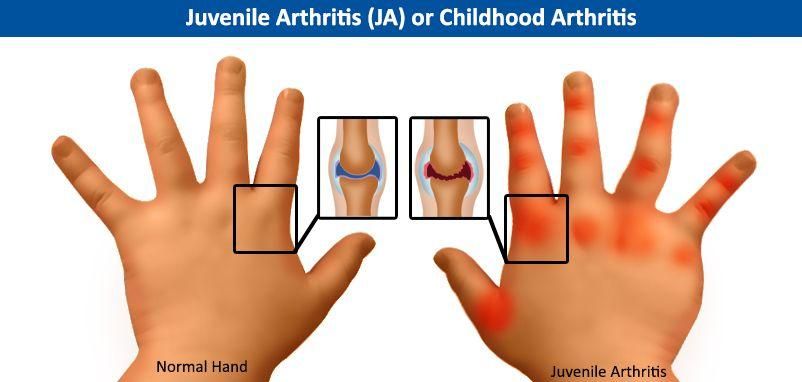
Juvenile arthritis is a disease in which there is inflammation (swelling) of the synovium in children aged 16 or younger. The synovium is the tissue that lines the inside of joints.
Juvenile arthritis is an autoimmune disease. That means the immune system, which normally protects the body from foreign substances, attacks the body instead. The disease is also idiopathic, which means that no exact cause is known. Researchers believe juvenile arthritis may be related to genetics, certain infections, and environmental triggers.
What are the different types of juvenile arthritis?
There are five types of juvenile arthritis:
• Systemic arthritis, also called Still's disease, can affect the entire body or involve many systems of the body. Systemic juvenile arthritis usually causes high fever and a rash. The rash is usually on the trunk, arms, and legs. Systemic juvenile arthritis can also affect internal organs, such as the heart, liver, spleen, and lymph nodes, but usually not the eyes. Boys and girls are equally affected.
• Oligoarthritis, also called pauciarticular juvenile rheumatoid arthritis, affects fewer than five joints in the first six months that the child has the disease. The joints most commonly affected are the knee, ankle, and wrist. Oligoarthritis can affect the eye, most often the iris. This is known as uveitis, iridocyclitis, or iritis. This type of arthritis is more common in girls than in boys, and many children will outgrow this disease by the time they become adults.
• Polyarthritis, also called polyarticular juvenile idiopathic arthritis (pJIA), involves five or more joints in the first six months of the disease -- often the same joints on each side of the body. This type of arthritis can affect the joints in the jaw and neck as well as those in the hands and feet. This type also is also more common in girls than in boys and more closely resembles the adult form.
• Psoriatic arthritis affects children who have both arthritis and the skin disorder psoriasis. The child might get either the psoriasis or the arthritis years before developing the other part of the disease. Children with this type of arthritis often have pitted fingernails.
• Enthesitis-related arthritis is a type of arthritis that often afflicts the spine, hips, eyes, and entheses (the places where tendons attach to bones). This type of arthritis occurs mainly in boys older than 8 years of age. There is often a family history of arthritis of the back (called ankylosing spondylitis) among the child's male relatives.
What are the symptoms of juvenile arthritis?
Children with juvenile arthritis can have no symptoms at all. Symptoms may also vary depending on the type of arthritis. Symptoms of juvenile arthritis may include:
• Joint stiffness, especially in the morning
• Pain, swelling, and tenderness in the joints
• Limping (In younger children, it may appear that the child is not able to perform motor skills he or she recently learned.)
• Persistent fever
• Rash
• Weight loss
• Fatigue
• Irritability
• Eye redness or eye pain
• Blurred vision
How is juvenile arthritis diagnosed?
Because a child may have no symptoms of juvenile arthritis, and because some of the symptoms can be associated with other diseases, a diagnosis may be difficult. Because there is no actual test for juvenile arthritis, the diagnosis is made by excluding other conditions that may cause similar symptoms, such as bone disorders or breaks, fibromyalgia, infection, Lyme disease, lupus, or cancer.
The doctor is likely to begin by taking a complete medical history and performing a complete medical exam. Additional testing might be useful in determining what type of arthritis the child has. Some of the other tests that might be ordered include:
• Complete blood count (white cells, red cells, and platelets)
• Lab tests on blood or urine
• X-rays (to rule out breaks or damage to bones)
• Imaging tests, such as magnetic resonance imaging (MRI) scans
• Blood culture to check for bacteria, which could indicate an infection in the bloodstream
• Tests for viruses
• Tests for Lyme disease
• Bone marrow exam, which is used to check for leukemia
• Erythrocyte sedimentation rate to see how quickly the red blood cells fall to the bottom of a test tube (The rate is faster in most people who have a disease that causes inflammation.)
• Test for rheumatoid factor, an antibody that may be found in people with arthritis (An abnormal result is more common in adults than in children.)
• Antinuclear antibody test to show evidence of autoimmunity (Autoimmunity is a disease state in which the body's defense system, the immune system, malfunctions and attacks the body itself. This test is also useful in predicting if eye disease will develop in children with juvenile arthritis.)
• Bone scan to detect changes in bones and joints (This test may be ordered if the symptoms include unexplained pain in the joints and bone.)
• Joint fluid sampling and synovial tissue sampling, which might be performed by an orthopedic surgeon
What is the treatment for juvenile arthritis?
Treatment for juvenile arthritis generally includes exercise, medications and physical therapy. The treatment plans are also based on the type of juvenile arthritis. For instance, children who have polyarticular juvenile arthritis and who have a positive result on the rheumatoid factor test have the potential for more joint damage and may need more aggressive treatment.
In general, though, treatment for juvenile arthritis has several main goals:
• To relieve pain
• To reduce swelling
• To increase joint mobility and strength
• To prevent joint damage and complications
The following types of drugs may be used to treat juvenile arthritis:
• Nonsteroidal anti-inflammatory drugs (NSAIDs) are used to treat pain and swelling. There are NSAIDs available over the counter and others that are prescription only. NSAIDs include products such as ibuprofen and naproxen. Possible side effects are nausea and stomach ache; these drugs should be taken with food. Aspirin is included in the NSAID category, but is rarely prescribed for treating arthritis.
• Slow-acting anti-rheumatic drugs (SAARDs) are used to treat pain and swelling over time and usually take several weeks or more to work. These drugs are also called disease-modifying anti-rheumatic drugs (DMARDs). The doctor may prescribe drugs in this category in combination with NSAIDs. Lab tests to check for possible side effects are usually necessary. One of the most commonly used DMARDs is methotrexate (Rheumatrex). Other DMARDs include hydroxychloroquine (Plaquenil), sulfasalazine (Azulfidine), and drugs that block tumor necrosis factor (TNF), also called anti-TNF drugs. Etanercept (Enbrel) and etanercept-szzs (Erelzi) are examples of anti-TNF medication used to treat juvenile arthritis.
• Corticosteroids are also used to treat pain and swelling. Sometimes, before any other treatment is tried, steroids are given as an injection into the affected joint. In certain cases, the doctor might prescribe oral steroids (taken by mouth), but these are generally avoided in children because of adverse side effects, which may include poor growth and weight gain.
• Antimetabolites are a type of drug that is an aggressive therapy aimed at helping reduce further joint damage and preserve joint function. The new drug Xatmep is an oral form of methotrexate that can be used to treat polyarticular juvenile idiopathic arthritis in pediatric patients, usually when NSAIDs have been proven to be ineffective.
WebMD Medical Reference Reviewed by Dan Brennan, MD
